Inhibitors and immune tolerance induction in hemophilia A
Immune Tolerance Induction (ITI) seems a feasible therapy to treat patients with haemophilia A that develop inhibitors to clotting. The working mechanism of ITI seems to be successful restoration of regulatory B cells. This was concluded in the thesis by Sarah Schep at UMC Utrecht who received her PhD degree on December 23, 2021.
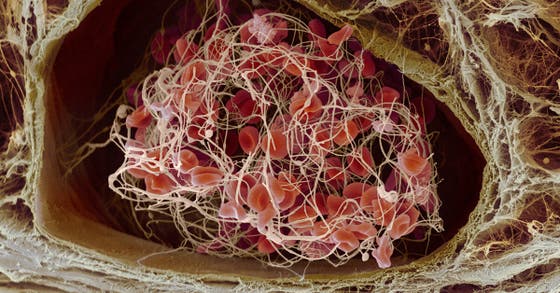
One of the main complications in the treatment of hemophilia A is the development of neutralizing antibodies against clotting factor VIII (FVIII), so called inhibitors. About 15-20 percent of people with hemophilia develop such an inhibitor that stops the clotting factors from being able to clot the blood and stop a bleeding. Hence treatment of bleeding episodes becomes extremely difficult, and the cost of care for a person with an inhibitor can skyrocket because more clotting factor or a different type of clotting factor is needed to control a bleeding. People with inhibitors often experience more joint disease and other problems from bleeding that result in a reduced quality of life.
The PhD research by Sarah Schep (Department of Hematology/van Creveld Clinic and Center for Translational Immunology, UMC Utrecht) was aimed at exploring mechanisms involved in inhibitor development as well as the eradication of inhibitors by means of Immune Tolerance Induction (ITI). According to the concept of ITI, repeated and long-term administration of FVIII (in a non-inflammatory state) ultimately results in downregulation of the immune response. The therapy is effective in 60-80 percent of all cases.
Immunoregulatory properties
Despite decennia of experience with ITI, data about FVIII-induced immunological changes during ITI is limited and deserve more exploration. The most significant findings from Sarah Schep’s research are that in a cross-sectional study inhibitor patients expressed a significantly lower frequency of regulatory B-cells (Bregs) and regulatory markers on CD4+ T-cells, which were restored by successful ITI. These findings suggest that an existing anti-FVIII immune response is associated with deficits in peripheral tolerance mechanisms and that Bregs and changes in immunoregulatory properties of CD4+ T-cells likely contribute to ITI in hemophilia A patients with inhibitors. A validation of these findings in a prospective study in previously untreated patients is currently ongoing.
Hemophilia A
Hemophilia A is an X-linked, recessive disorder caused by deficiency of functional FVIII, which may be inherited or arise from spontaneous mutation. The development of inhibitory alloantibodies to FVIII can severely complicate the treatment of genetic cases. Rarely, development of autoantibodies to FVIII results in acquired hemophilia A. Depending on the level of FVIII activity, patients with hemophilia may present with easy bruising; inadequate clotting of traumatic or even mild injury; or, in the case of severe hemophilia, spontaneous hemorrhage. Hemophilia A affects approximately 1 in 5.000 males, of which at least half suffers from severe disease.
PhD defense
Sarah Schep (1987, Gorinchem) defended her PhD thesis on December 23, 2021 at Utrecht University. The title of her thesis is “Inhibitors and immune tolerance induction in hemophilia A – a balancing act”. Supervisor was prof. dr. Roger Schutgens (Department of Hematology/van Creveld Clinic, UMC Utrecht) and prof. dr. Jan Voorberg (Sanquin and University of Amsterdam). Co-supervisors were dr. Marianne Boes (Center for Translational Immunology, UMC Utrecht) and dr. Kathelijn Fischer (Department of Hematology/van Creveld Clinic, UMC Utrecht). Sarah Schep has started a Fellowship Hematology at UMC Utrecht which is expected to be completed in April 2022.
