Jan 16: Systemic and tissue neutrophil responses to experimental trauma

Changes in neutrophil response (both count and characteristics) are often seen in people with severe (poly-)trauma. Experimental trauma surgery models have confirmed the effect of trauma on the count and presence of neutrophil subtypes in the blood, bone marrow and pulmonary tissue. These insights in the inflammatory response after trauma may form the basis for novel treatments and guidelines, resulting in improved outcome of trauma patients. These were the main conclusions by Michel Teuben (UMC Utrecht) who defended his PhD thesis on January 16.
Neutrophils are the most abundant type of circulatory white blood cells (normally 60-70 percent of all leukocytes). Neutrophil activation can be triggered by stimuli such as bacterial invasion, obstruction of vessels, fractures or organ injuries. Upon major trauma, or following myocardial infarction, a pathological neutrophil response (such as progressive neutropenia and increased heterogeneity of the blood neutrophil pool) can occur. Such changes may form the basis for life threatening complications like organ failure. Furthermore, they may also lead to impaired wound or fracture healing in trauma cases.
Aberrant neutrophil presence
The thesis by Michel Teuben- of which the research has primarily been performed at the Department of Traumatology, UMC Utrecht and the Department of Traumatology, University Hospital Zurich - demonstrates that prolonged surgery (>60 minutes) for trauma is associated with aberrant neutrophil presence in blood. To be more precise, the total number of circulatory neutrophil drops significantly after 60 minutes of surgery. Moreover, the number of a specific subtype of neutrophils, which are normally virtually absent, rises during ongoing surgery. These findings could form a first pathophysiological background for the ‘Damage Control Surgery´-concept.
In additional experiments by Teuben and colleagues it was shown that during these post-traumatic neutrophil alterations, the pulmonary as well as the bone marrow neutrophil populations also change markedly. Furthermore, in the case of isolated fractures, both blood and pulmonary neutrophil populations differ from healthy conditions for as long as two weeks. It was further shown that the applied treatment strategy for fracture fixation affects the viability of neutrophils in fracture hematoma.
These novel insights may form the basis for novel treatment modalities and guidelines, resulting in improved outcome of trauma patients.
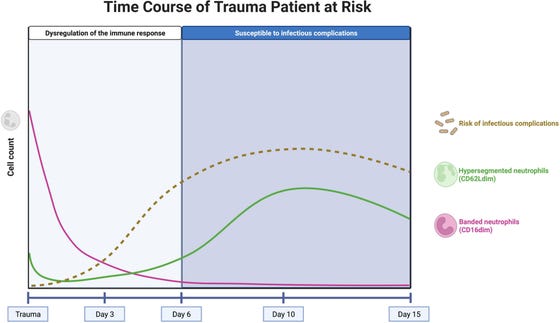
Concept of the neutrophil subset response over time in a trauma patient at risk for infectious complications. The pink line represents the course of well-functioning banded neutrophils, entering the circulation immediately after trauma. The green line represents the course of hypersegmented neutrophils, with impaired killing capacity. The brown, dashed line represents the risk of infectious complications over time. The risk increases after 3–5 days, when there are no banded neutrophils left in the circulation (de Fraiture et al. Front Immunol 2022).
Trauma
Major trauma –the 6th leading cause of death worldwide and a major cause of disability- is any injury that has the potential to cause prolonged disability or death. There are many causes of major trauma, including falls, motor vehicle collisions, stabbing wounds, and gunshot wounds. Depending on the severity of injury, quickness of management, and transportation to an appropriate medical facility (called a trauma center) may be necessary to prevent loss of life or limb. Approximately 80 percent of fatalities after major (poly)trauma occur within 4 hours after the accident. The remaining 20 percent occurs in days or weeks after the accident, mainly as a result of tissue damage related inflammatory complications such as sepsis or multiple organ failure (de Fraiture et al. Front Immunolo.
PhD defense
Michel Teuben defended his PhD thesis on January 16, 2023 at Utrecht University. The title of his thesis is “Systemic and tissue neutrophil responses to experimental trauma”. Supervisors were prof. dr. Luke Leenen (Department of Traumatology, UMC Utrecht), prof. dr. Leo Koenderman (Center for Translational Immunology, UMC Utrecht) and prof. dr. Hans-Christophe Pape (Department of traumatology, University Hospital, Zürich, Switzerland). Michel works as a trauma surgeon at the University Hospital, Zürich, Switzerland.
