Newly described mechanism offers opportunities for treatment of cystic fibrosis
People with cystic fibrosis have a compromised defense against pathogens in the lungs, due to the accumulation of thick mucus in their lungs in which pathogens thrive. Apart from the mucus, the fluids lining the airway surfaces are also too acidic and that inhibits additional antimicrobial defense mechanisms against pathogens. Researchers from Newcastle University and University Medical Center Utrecht have described a new cellular mechanism that influences this acidity using miniature airways, and discovered two already approved drugs that could potentially be used to change the acidity in people with CF.
Lees artikel in het Nederlands >
Cystic fibrosis (CF) is a hereditary disease that can be caused by many different mutations in a single gene in the DNA called CFTR. These mutations disrupt the function of the CFTR protein that is produced from this part of the DNA. Reduced CFTR function leads to changes in transport of salts and fluids in the cells that line the airway, leading to a different composition of the fluids in the airways and result in the classic thick and tough mucus that is a hallmark of the disease.
Tougher but also more acidic
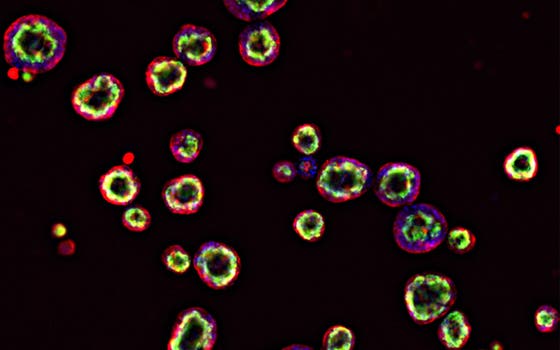
But in addition to tough mucus, the airway surface fluid also becomes more acidic, which reduces bacterial killing by antimicrobial molecules made by airway cells. The mucus builds up and bacterial infections become more common. Aided by a Strategic Research Consortium award from the Cystic Fibrosis Trust, researchers from University Medical Center Utrecht and Newcastle University have now found new molecular mechanisms in miniature airways from people with CF, that contribute to the acidification of the airway surface fluid.
Involved researcher Gimano Amatngalim of the Regenerative Medicine Center Utrecht, part of UMC Utrecht, explains the value of these molecular channels: 'We investigated whether other channels can stop the acidification of the airway surface fluid. We studied this by genetically disabling these channels with CRISPR technology in cultured mini-airways of people with CF. As a result, we have discovered that when the specific SLC26A4 anion exchanger is disabled, the acidity is further reduced in the mucous membrane of people with CF.'
A new mechanism offers opportunities for treatment
The mechanisms described around the SLC26A4 exchanger offer potential for a new treatment. If a drug could influence the mechanism, the acidity of the mucous membrane might also be controlled. This would provide a new treatment mechanism for CF that is independent of the CFTR channel. This independence is interesting because current medications against CF only act on the CFTR channel. But some people with CF lack this CFTR channel and therefore cannot be treated with current medications.
The researchers tested approved drugs on the airway models and found two possible candidates. Amatngalim: 'Because those two drugs have already been approved, they could be tested relatively quickly in people with CF.'
Building on previous discoveries
This research builds on research that has already led to major improvements for people with CF. About ten years ago, UMC Utrecht professor Jeffrey Beekman developed a test based on intestinal organoids from people with CF, which can quickly and accurately predict which of the many medications are effective for the specific form of cystic fibrosis that a person has. This provides faster and more appropriate treatment for many patients and reduces the waste of often expensive medicines. “By using respiratory organoids now, we get a better picture of the complexity of the disease in the respiratory tract than with intestinal organoids,” says Beekman.
